Abstract
Background. Increasing numbers of adolescent and young adult (AYA) with acute leukemia (AL; acute myeloid leukemia [AML] and acute lymphoblastic leukemia [ALL]) are transitioning to long-term survivorship following allogeneic hematopoietic cell transplantation (HCT) and are at risk for certain morbidities after HCT due to myeloablative conditioning (MAC) with total body irradiation (TBI) or non-TBI-based chemotherapy (CT). Using data from the Center for International Blood and Marrow Transplantation Research (CIBMTR), we evaluated late effects (LEs) following MAC HCT and furthermore compared the effect of TBI vs. CT-based MAC on LEs and overall survival (OS) in a large cohort of one-year disease-free AYA survivors following HCT for AL. We hypothesized that the use of TBI, relative to CT-based MAC, would lead to equivalent long-term survival in this population but that TBI conditioning would be associated with significantly increased LEs following HCT.
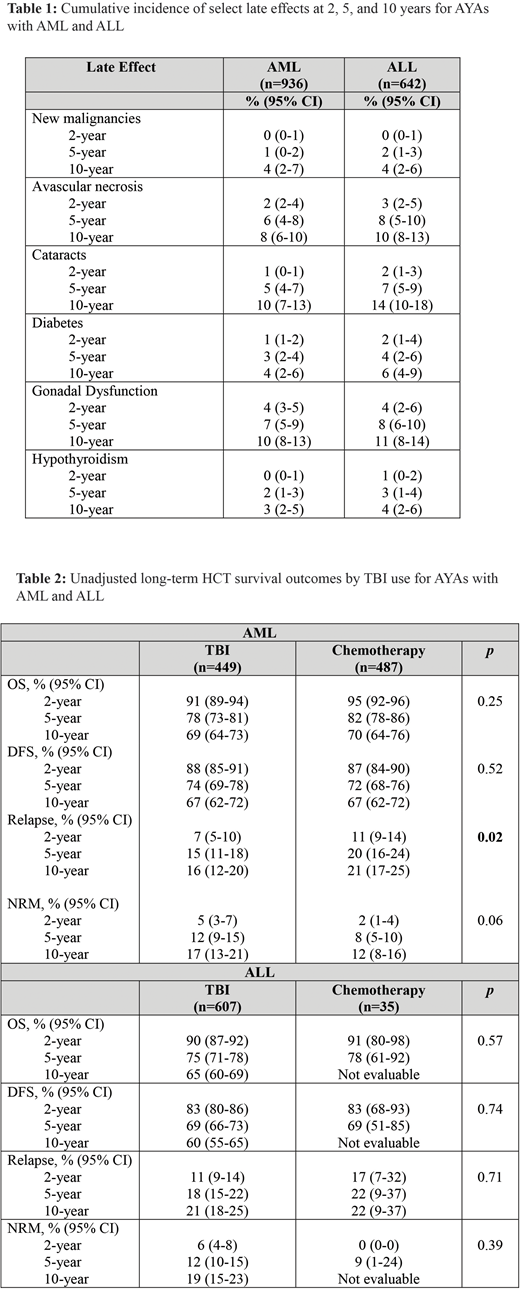
Methods. AYAs (ages 15-39 years at HCT) with AL who received first MAC HCT between 2000-2014 from a HLA matched sibling or 8/8 matched unrelated donor (MUD) and were alive and disease-free at one year following HCT were included. The cumulative incidence (CI) of LEs (avascular necrosis [AN], cataracts, congestive heart failure, myocardial infarction, diabetes [DM], gonadal dysfunction, growth disturbance, hypothyroidism, pancreatitis, renal failure requiring hemodialysis, and strokes/seizures) was estimated at 2, 5 and 10 years after HCT, with death as a competing risk. Multivariable Cox proportional hazard models evaluated patient and HCT risk factors, including the main effect of TBI vs. CT-based MAC, for the most frequently occurring LEs (limited to AML cohort only as majority of ALL patients received TBI) and for OS.
Results. The study population included 1,578 one-year disease-free AYA survivors of AML (n=936) or ALL (n=642) who received first MAC HCT with TBI (AML: 449; ALL: 607) or CT (AML: 487; ALL: 35). The median TBI dose was 1200 cGy (range, 550 - 1800). The median age at HCT for AML and ALL was 29 and 26 years, respectively. The majority were male (AML: 54%; ALL: 67%), transplanted in first complete remission (AML: 62%; ALL 59%) with MUD donors (AML: 56%; ALL 55%), and had GVHD prophylaxis consisting of a calcineurin inhibitor and methotrexate (AML: 83%; ALL 83%) without T-cell depletion. The most common TBI and CT-based MAC regimens were TBI/cytoxan and busulfan/cytoxan, respectively. Median follow-up (months) of survivors was 82 (range, 12-194) for AML and 92 (range, 12-194) for ALL. The estimated CI of LEs in AML and ALL patients are shown in Table 1. Multivariable analyses for individual LEs in the AML cohort showed that CT- based MAC was independently associated with a lower risk of cataracts (HR 0.19, 95% CI 0.10 - 0.37). There was no significant association between TBI and secondary malignancies, DM, gonadal dysfunction, or hypothyroidism. cGVHD was independently associated with significantly increased risk of cataracts (HR 2.88, 95% CI 1.58 -5.24), AN (HR 2.55, 95% CI 1.25 - 4.07), and DM (HR 2.85, 95% CI 1.05 - 7.73). Unadjusted long-term HCT survival outcomes for AYAs with AML and ALL did not significantly differ based upon TBI vs. CT-based MAC (Table 2) despite significantly higher disease relapse among the CT cohort (AML only). Limited and severe cGVHD occurred in 12% and 51% of AML patients, respectively, and 13% and 53% of ALL patients, respectively, and did not differ by conditioning. In multivariable analyses for OS, HCT in relapse (HR 2.40, 95% CI 1.59 - 3.63), poor-risk cytogenetics (HR 2.09, 95% CI 1.24 - 3.52), peripheral blood stem cell graft (HR 1.46, 95% CI 1.07 - 1.97), cGVHD (HR 1.36, 95% CI 1.04 - 1.80), and a new malignancy post-HCT (HR 4.40, 95% CI 2.21 - 8.74) were associated with significantly inferior OS in AML. Undergoing HCT in CR2 (HR 1.50, 95% CI 1.09 - 2.07) or in relapse (HR 3.67, 95% CI 2.31 - 5.82), and a new malignancy post-HCT (HR 3.11, 95% CI 1.26 - 7.68) were associated with significantly inferior OS in ALL.
Conclusion. AYAs with AL who are disease-free survivors at one-year have favorable long-term HCT outcomes. Long-term survival in this population appears unrelated to a TBI vs. CT-based MAC regimen. Development of cataracts is increased in long-term AYA AML HCT survivors receiving TBI-based MAC. Screening for LEs is important in survivors of AYA HCT for AL, regardless of the use of TBI or CT- based MAC regimens.
Muffly:Shire Pharmaceuticals: Research Funding; Adaptive Biotechnologies: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal